Current Research in Emergency Medicine
[ ISSN : 2832-5699 ]
Cancer and Matters of The Heart: Cardiac Metastases and The Potential Presentation to the Emergency Department
1Senior Consultant, Department of Emergency Medicine, Singapore General Hospital, Singapore
2Professor, Dukes-NUS Graduate Medical School, Yong Loo Lin School of Medicine, National University of
Singapore, Singapore
3Director, SingHealth Duke NUS Institute of Medical Simulation, Singapore
Corresponding Authors
Keywords
Abstract
Cardiac metastases are relatively rare. However, over the years, as diagnostics and therapeutics of cancer management improve, cancer patients are living longer. The longer survivality means there may be more metastatic disease as well as later stage disease. Scanning for cardiac metastases is not routine practice for patients with malignancies and is not currently a recommendation is most guidelines. It is still an assessment on a case by case basis. Thus, the need for high vigilance and awareness is assessing patients’ symptomatology and presentation. The spectrum of presentation of cardiac metastases is wide and varied and some common ones are shared in this paper. This ranges from symptoms such as fatigue, shortness of breath, fainting, hypotension, heart failure, cardiac murmurs and arrhythmias and others. Despite the fact that patients presenting with such a spectrum are common, not often are they firstly attributable to cardiac metastases. This is the reason why in predisposed patients, the treating physicians or emergency physicians must sought deeper into the background history, extend of cancers and have a high index of suspicion in order not to miss the diagnosis and to start the ball rolling in terms of ordering the most suited investigations.
Introduction
In general, cardiac metastases are rare. However, as the incidence of cancer rises, cardiac metastases is gaining more diagnostic and therapeutic importance. One of the first cases to be reported in the literature was in 1700 by Boneti [1]. This was followed by a few more reports in the 1800s and then into the 1900s [2-9]. Potentially, almost every cancer can spread to the heart. These cases are often difficult to diagnose due to the fact many may not have symptoms at all, whilst the rest may have late symptoms or present with health failure and arrhythmias, where cardiac metastasis is usually not considered in the first line diagnosis. Sometimes, the metastasis is incidentally discovered, during the course of working up patients, who may have a wide range of clinical presentations. Echocardiography, which is commonly used in the initial, non-invasive assessment of cardiac structure and function, has frequently been one of the first investigations to point to a possible cardiac metastasis [10-12]. In the past, it was believed that cardiac metastases represent a rare phenomenon. The reasons for this belief were [13-15]:
a. The perception that heart tissue was not receptive to tumour cells ‘seeding’.
b. The kneading action of the striated heart muscles reduces the likelihood tumour cells ‘seeding’.
c. The rapid blood flow and turbulence within the heart chambers.
Today, we know the above reasoning are inaccurate. In fact, practically almost every tumour has been reported in
cardiac metastases cases. Some common primary cancers with cardiac metastases include lung cancer, breast cancer,
leukemia, lymphoma, mediastinal tumours, head and neck cancers and melanoma [11,12, 16, 17].
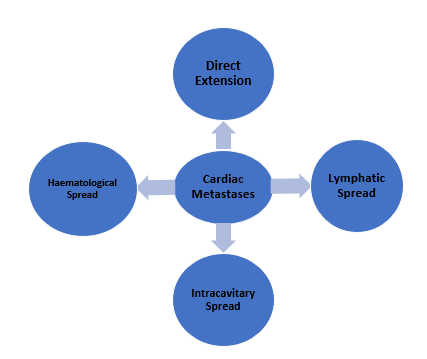
Modes of Spread (Figure 1)
Cancer cells most often reach the heart via the haematogenous route, but there are others ways through which the spread can happen. Cancer has been postulated to be able to spread to the heart by one of the following mechanisms [1, 11,14, 18]:
a. Direct extension: especially in patients where the cancer is within the thorax, in the mediastinum or adjacent to the heart (eg. lung cancers)
b. Haematological spread: this is by means of embolic tumour cells reaching the heart through the coronary vessels,through which they then invade the heart.
c. Lymphatic spread: malignant cells reach the heart by the retrograde flow through the mediastinal and tracheabronchial lymphatic channels. This may sometimes be seen in the context of lymphangitis carcinomatosis (whereby the lymphatic channels of the heart are filled with malignant cells).
d. Intracavitary spread via diffusion from the inferior vena cava and pulmonary veins (this happens when fibrin forms on tumour cells which are free and floating in the venous system, which then supports further growth of the tumour and this tumour thrombus may then extend into the chambers of the heart.
Within the structure of the heart itself, metastases have been known to affect the pericardium, epicardium, myocardium, endocardium as well as the heart chambers. Tumour from the myocardium can spread to the epicardium and pericardium. Tumour cells can also be carried via retrograde lymphatic flow through the bronchomediastinal lymph channels to the myocardium. In fact, “seeded” metastatic cells in any part of the heart can spread to adjacent structures (e.g. from myocardium to pericardium) [15, 18, 19]. Considering, all these possibilities, it is not easy for the Emergency Physician to make the diagnosis of cardiac metastasis first line. Often, they will have to sieve through the history to assess if there is a background of cancer, which types of cancer and what is the primary site or extend of the disease. Following this, a series of investigations will be required in order to confirm the diagnosis.
Figure 1: Modes of Spread of Cardiac Metastases
Possible Emergency Department (ED) Presentation
With the wide spectrum of primary cancers that can metastasize to the heart as well as the different anatomical areas and structures of the heart that can be involved, one can imagine that the potential presentation to the ED too will be very broad ranging. Symptoms such as giddiness, fainting, fatigue, shortness of breath, chest discomfort and exertional fatigue are all very generic and non-specific. Table 1 represents some potential clinical presentations which may be encountered in the ED. It may appear obvious that these range of symptoms are many and varied and can tend to overlap with other diagnoses. The diagnosis of cardiac metastases would likely not be first in the minds of Emergency Physicians (EPs), until they have ruled out more common differentials. At Singapore General Hospital, which is part of an Academic Medical Centre, housing The National Cancer Centre, frontline physicians need to be vigilant and bear this in mind, in view of the fact that our cancer patient load is very high. Having a cancer specialist centre as this on site means cancer-related complications can present to our ED. Also, with the extended survival of oncologic patients today, due to improved diagnostics and therapeutics, many may live longer and develop complications and metastases. One unique consideration when dealing with the heart is to understand that it is incapable of mending injured or damaged tissue. This is because cardiac myocytes are terminally differentiated; which means they do not re-enter the cell cycle to proliferate and repair damaged tissues. This is an interesting point to note in managing cardiac lesions as well as cardiac secondaries. In a study of 1029 autopsy cases by Klatt et al, it was noted that:
-Lung cancer was the commonest primary site cancer
-Adenocarcinoma was the commonest cell type metastases
-The epicardium was involved I 75.5% of metastatic lesions
-In cases of lymphoma, they were associated with acquired immune deficiency
syndrome
Table 1: The Potential Clinical Presentation in the ED versus the Sites of Cardiac Metastases
|
Clinical Presentation |
Site/s of Cardiac Metastases |
|
Hypotension, hemodynami c instability |
Ventricular outflow tract obstruction from tumour metastasis or reduction of the flow
Significant sized pericardial effusion or pericardial tamponade |
|
Arrhythmia |
Epicardial, myocardial and endocardial metastases |
|
Chest pain, pleuritic chest pain |
Metastases within the mediastinal and thoracic cavity |
|
Angina Acute Coronary Syndrome Myocardial Infarction
Coronary Artery Disease |
Tumour emboli reaching the heart through the coronary vessels; thus potential to obstruct coronary arteries causing angina
Haematological spread or direct spread by cancer cells invading the heart |
|
Dysphagia
Dyspnoea
|
Metastases causing pressure symptoms in the mediastinal structures adjacent to the heart eg. esophagus, airway structures such as bronchus, bronchioles |
|
Cerebro-vascular Syndromes |
Tumour embolization ( from the heart chambers to the brain circulation) |
|
Heart Failure |
Metastases to myocardium or structures in the heart eg. valves |
|
Valvular Dysfunction |
Metastases to the valves |
|
Pericarditis, Pericardial effusion Constructive pericarditis is rare in metastases Chronic Pericarditis can occur |
Metastases to the pericardium |
|
Electrocardiography Changes: ST and T wave changes |
Metastases affecting the conduction system/ tissue
|
Investigations and Management
How EPs order investigations for such patients is prompted by their symptoms and signs. Usually the patients would have gone through a series of investigations for their primary cancer work-up. Sometimes, for those who remain asymptomatic, cardiac metastases are picked up during routine tests and screening. One of the common test that can suggest cardiac metastases is heart echocardiography. This is often used as a screening cardiac function test, which can also assess valvular and ventricular competence, identify any intra-ventricular or cardiac chamber masses and pickup structural wall abnormalities. The diagnostic accuracy can be as high as 80% for an initial screening tool for cardiac metastases, but it is also operator dependent. The more experienced the person performing the echocardiographic studies, the higher the likelihood of picking up even smaller abnormalities. It is also important to note that often the test is being done for other reasons but incidentally picks up the suspected cardiac metastases [19, 20-22]. Other investigations such as Cardiac Ultrasound (CUS), CT Scan and magnetic resonance imaging (MRI) are also useful for further definition and confirmation. Cardiac MRI provides excellent contrast resolution and can show great details of the distribution of tumour as well as differentiate it from myocardium or thrombus, compared to CUS and CT Scan of the heart. MRI also gives better definition of the surrounding structures, which is crucial in the assessment of spread. PET (Positron emission tomography) scans are at times used because it is part of the armamentarium of tests for working up the primary cancer, such as head and neck cancers [20,21]. Chest Xrays are usually non-specific and may show cardiomegaly and at times, prominence of the azygous vein if pericardial effusion is present. A big challenge in diagnosing cardiac metastases is to differentiate these from primary cardiac tumour such as myxoma. Thus, very good quality, high resolution imaging can be very helpful [12, 17, 19].
There is no standard or fixed treatment for cardiac metastases. As it is, it is already quite rare and when detected in cancer patients, it often means the disease is at a late or advanced stage. These patients are usually not good surgical candidates due to a variety of reasons such as the site of the metastases, the extent of their disease process as well as medical fitness for operation (many of these patients have multiple co-morbidities which put them at higher risk) [23].
Discussion
Cardiac metastases are relatively rare in occurrence, but that does not mean it does not occur. Thus, in analysing patients’ symptoms and presentation, after considering the more common first line diagnoses, thinking about these rarer causes is useful. It requires EPs to avoid fixations and think broad spectrum, especially as we have seen that the presentation with cardiac metastases can be wide-ranging. Understanding about the primary cancer is very helpful, just as knowing the extend of disease spread is. We have learnt and made observations from both post-mortem (especially in the early years) as well as clinical cases and sharing with the medical fraternity helps remind us of these rarer possibilities. Currently, scanning for cardiac metastases is not routine practice for patients with malignancies and is not a recommendation is most guidelines. It is still an assessment on case by case basis.

Figure 2a: ED presentation with shortness of breath in a patient with left sided cancer of the lung (non small cell lung cancer). The chest Xray shows opacification of he left hemihorax

Figure 2b: CT Scan showing left hilar mass extending into the left atrium
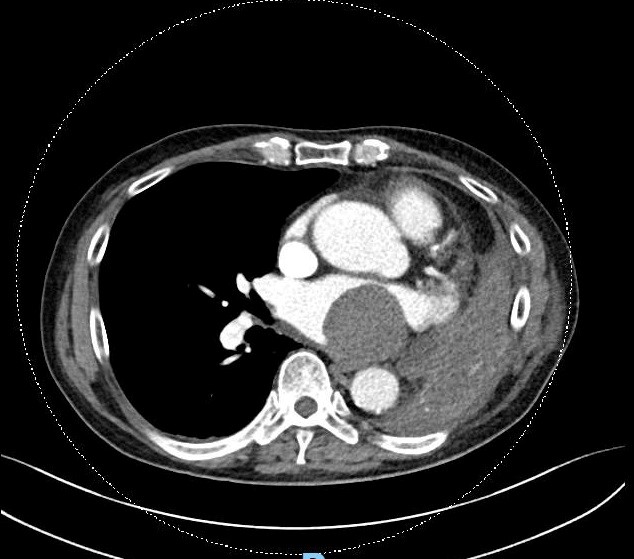
Figure 2c: CT Scan cut in cross-section showing the mass (cancer) in the left atrium
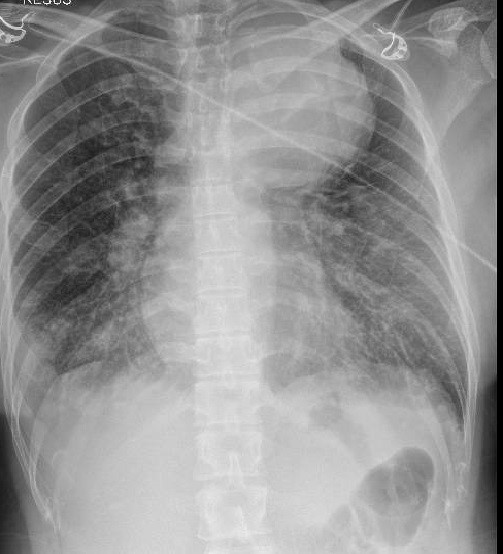
Figure 3a: Large opacity in the left upper hemithorax in a patient with history of cancer of the breast 5 years prior to presentation. There are features of lymphangitis carcinomatosis on the Chest Xray, especially in the lower zones
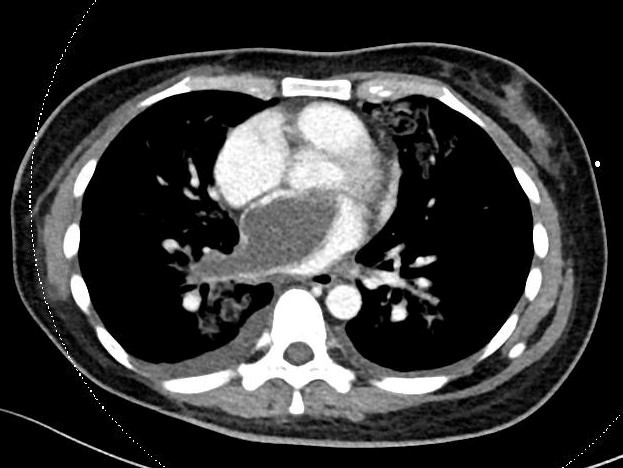
Figure 3b: Cross-sectional CT Scan cut showing a large filling defect in the left atrium extending into the right inferior pulmonary vein

Figure 3c: The filling defect (metastasis) in the left atrium extending to the pulmonary veinon CT Scan
Conclusion
Cardiac metastases can be considered quite rare. However, it is important to think about this especially, in particular when there are no other good explanation to explain the cardiac related symptoms.
On the other hand, there are also not many centres that have an established protocol for soughting out cardiac metastases, as in looking for liver, lung, brain and bone metastases. Thus a high index of suspicion is useful in the appropriate case presentation.
References
- Tedeschi A (1893) Beitrag zum Studium der Herz-geschwulste (Translation: Contributions to the study of cardiac tumours). Prag med wchnsch 18: 121.
- Coates BH (1822) Case of a singular tumour within the vena cava and attached to the Eustachian valve. Philadelphia JM and Phys Soc 4: 334.
- Burke EM (1934) Metastatic tumours of the heart. Am J Cancer 20: 33.
- Nusbaum WD, Heyer FW (1935) Carcinoma metastases to heart and subcutaneous tissues. Am J Cancer 24(4): 831-838.
- Fishberg AM (1930) Auricullar fibrillation and flutter in metastatic growths of right auricle. Am J M Sc 180: 629.
- Lisa JR, Hirschhorn L, Hart CA (1941) Tumours of heart. Report of 4 cases: Review of literature. Arch Int Med 67(1): 91-113.
- Morris LM (1927) Metastases to heart from malignant tumours. Am Heart J 3: 329.
- Prichard RW (1951) Tumours of heart: review of subject and report of 150 cases. Am J Cancer 27: 329.
- Smith DS (1937) Neoplastic involvement of the heart: 2 cases diagnosed before death. JAMA 109(15): 1192-1194.
- Bussani R, DeGiorgio F, Abbate A, Silvestri F (2007) Cardiac metastases. J Clin Pathology 60(1): 27-34.
- Strecker T, Rosch J, Weyand M, Agaimy A (2012) Primary and metastatic cardiac tumours: characteristics, surgical treatment and histological spectrum: a ten year experience of a German Heart Centre. Cardiovascular Pathology 21(5): 436-443.
- Neragi-Miandoab S, Kim J, Vlahakes GJ (2007) Malignant tumours of the heart: a review of tumour type, diagnosis and therapy. Clin Oncol 19(10): 748-756.
- Tsai YT, Kuo SW, Hao SP (2010) Cardiac tamponade: a rare presentation from a rare metastatic site in oral squamous cell carcinoma. Eur Arch Otorhinolaryngol 267(9): 1483-1485.
- Werbel GB, Skom JH, Mehlman D, Michaelia LL (1985) Metastatic squamous cell carcinoma to the heart. Unusual cause of angina decubitus and cardiac murmur. Chest 88(3): 468-469.
- Kim JK, Sindhu K, Bakst RL (2019) Cardiac metastasis in a patient with head and neck cancer: a case report and review of the literature. Case Rep Otolaryngol 2019: 9581259.
- Agrawal Y, Nazroo J-YR, Khan BA, DeGregorio M (2019) Transmural cardiac metastasis of lung cancer with biventricular mobile extensions presenting as ST-elevation. BMJ Case Rep 12(10): e232571.
- Klatt EC, Hertz DR (1990) Cardiac metastasis. Cancer 65(6): 1456-1459.
- Lichtenberger JP, Reynold OA, Keung J, Keung E, Carter EW (2016) Metastasis to the heart. A Radiological approach to diagnosis and pathological correlation. AJR Am J Roentgenol 207(4): 1764-1772.
- Goldgerg AD, Blankstein R, Padera RF (2013) Tumour metastasis to the heart. Circulation 128(16): 1790-1794.
- Burazor I, Aviel-Roven S, Imazo M, Goitein O, Perelman M, et al. (2018) Metastatic cardiac tumour: from clinical presentation through diagnosis to treatment. BMC cancer 18(1): 202.
- Bilani N, Elson L, Martinez F, Badler D, nahleh Z, Eliminian E, Alley E (2020) A multi-modal approach to evaluate cardiac metastasis in a case of non small cell lung cancer. Case Report Oncol 13(1): 212-218.
- Bogren HG, Demaria AN, Mason DT (1980) Imaging procedure in the detection of cardiac tumours with emphasis on echocardiography: a review. Cardiovascular Interven radiology 3(3): 107-125.
- Vlachostregos P, Daliana D, Papandreaou C (2012) Basic concepts in metastatic cardiac disease. Cardiol Res 3(2): 47-48.
Citation: Lateef F (2022) Cancer and Matters of The Heart: Cardiac Metastases and The Potential Presentation to the Emergency Department. Curr Res Emerg Med 2: 1035