Current Research in Emergency Medicine
[ ISSN : 2832-5699 ]
Co-infection of COVID-19 and Monkeypox: A Case Report from Florida, USA, 2022
1Charles E. Schmidt College of Medicine, Florida Atlantic University, Boca Raton, Florida, USA
2Baptist Health Boca Raton Regional Hospital, Boca Raton, Florida, USA
Corresponding Authors
Keywords
Abstract
Monkeypox is a re-emerging zoonotic disease of the orthopoxvirus genus presenting with myocutaneous symptoms similar to those caused by smallpox. Patients infected with monkeypox may experience a prodromal period with flulike symptoms lasting between 1-4 days, an asymptomatic incubation period lasting 7-17 days and a symptomatic rash period lasting 14-28 days between the appearance of widespread vesiculopapular lesions and desquamation. Specific risk factors for the current monkeypox outbreak include HIV infection, prior STI infection, male sex, young-adult age (specifically being in the 20’s-30’s age group), engaging in risky behaviors (such as unprotected sex) and men having sex with other men. We report the case of a 38-year old HIV+ patient testing positive for monkeypox, COVID-19 and herpes who presented to the emergency department with widespread vesiculopapular lesions. One week prior to ED presentation, the patient experienced flu-like symptoms including fever and, two days later, developed a vesiculopapular rash beginning on his face and spreading downwards to his extremities, trunk and genitalia. The flu-like symptoms developed twelve days after attending an event where the patient reported having sex with multiple other men. The patient was treated with intravenous fluids and supportive care alongside his HIV medications. Nine days after initial ED presentation, all skin lesions were desquamated and the patient was discharged from the hospital. To our knowledge, this is one of the first reported cases of co-infection with COVID-19 and monkeypox in Florida and the United States more broadly. Despite our patient’s several risk factors for monkeypox infection, and immunosuppressed status, he experienced an uncomplicated clinical course. As vaccination and antiviral treatments become more available for monkeypox patients, our case suggests supportive care with airborne and contact precautions may be adequate in the treatment of future monkeypox patients where these treatments are unavailable.
Introduction
Monkeypox is a reemerging zoonotic disease of the orthopoxvirus genus with myocutaneous symptoms similar to those caused by smallpox [1-3]. This virus, first identified in captive monkeys, originates in Central and Western Africa with reservoirs in mammals including humans [1]. Patients may experience an incubation period of 7-17 days, prodromal period of 1-4 days with fever along with generalized headache, fatigue and a symptomatic rash period lasting 14-28 days between lesion appearance and desquamation [2]. Known mechanisms of transmission include large respiratory droplets, infected bodily fluids, and contact with skin lesions [4,5]. The monkeypox virus shares many common antigenic and structural features with smallpox, leading to a significant cross-immunity between the viruses. Accordingly, the eradication of smallpox has increased immunological susceptibility to monkeypox infection via the decline in cross-immunity from smallpox infection and/or vaccination [6]. Specific risk factors for the current monkeypox outbreak include HIV infection, prior sexually-transmitted infection, male sex, youngadult age, engagement in risky behaviors (such as unprotected sex) and men having sex with other men [7].
Herein, we report a case of a 38-year old living with HIV with widespread vesiculopapular lesions who tested positive for SARS-CoV-2 in the Emergency Department (ED). This patient was later confirmed to have contracted monkeypox via PCR testing performed at the health department. This case highlights the management of an immunosuppressed patient with multiple comorbidities who presented with lesions suggestive of monkeypox viral infection.
Case Presentation
A 38-year-old homeless man with a history of HIV, herpes and intravenous drug use presented to the ED with a chief complaint of COVID-19 symptoms and a rash. Eight days prior to ED presentation, the patient was admitted to a drug rehabilitation center and developed fever, chills, fatigue, malaise, myalgia and a non-productive cough the following day. Six days prior to ED presentation, he developed a vesiculopapular rash beginning on his face and spreading downwards to his extremities, trunk and genitalia, associated with pain in the genital region. The patient attended a large outdoor social gathering in New York City three weeks prior and reported having sex with multiple other men during the event. He has a history of HIV infection treated with an emtricitabine, rilpivirine and tenofovir alafenamide fixed-dose combination tablet and dolutegravir and past use of substances including gamma hydroxybutyrate, ketamine and methamphetamine. The patient was unvaccinated for SARSCoV-2 and was unable to confirm any past infections with this virus.
On physical exam, the patient was alert and oriented to person, place, and time upon arrival to the ED. He was afebrile (37°C) and in some discomfort with a heart rate of 84 beats per minute, blood pressure of 128/64 mmHg, and 18 respirations per minute. The patient had tonsillar inflammation, but no cervical or axillary lymphadenopathy. Heart and abdominal exams were normal. The pulmonary exam had pertinent negatives of no cough or shortness of breath with lungs clear to auscultation and a SpO2 of 97%. Physical exam was significant for dry mucous membranes and skin with scattered vesiculopapular lesions on his face, torso (Figure 1A), extremities (Figure 1B) and genitalia. The patient’s oral mucous membranes, palms, and soles were spared. On ED admission, the patient tested positive for SARS-CoV-2, had an elevated white blood cell count of 13,200 cells per microliter of blood (Reference Range: 4,500-11,000 cells per microliter of blood) and was later confirmed to have contracted monkeypox via PCR testing. His laboratory results were otherwise insignificant with a normal CD4+ T-cell count.
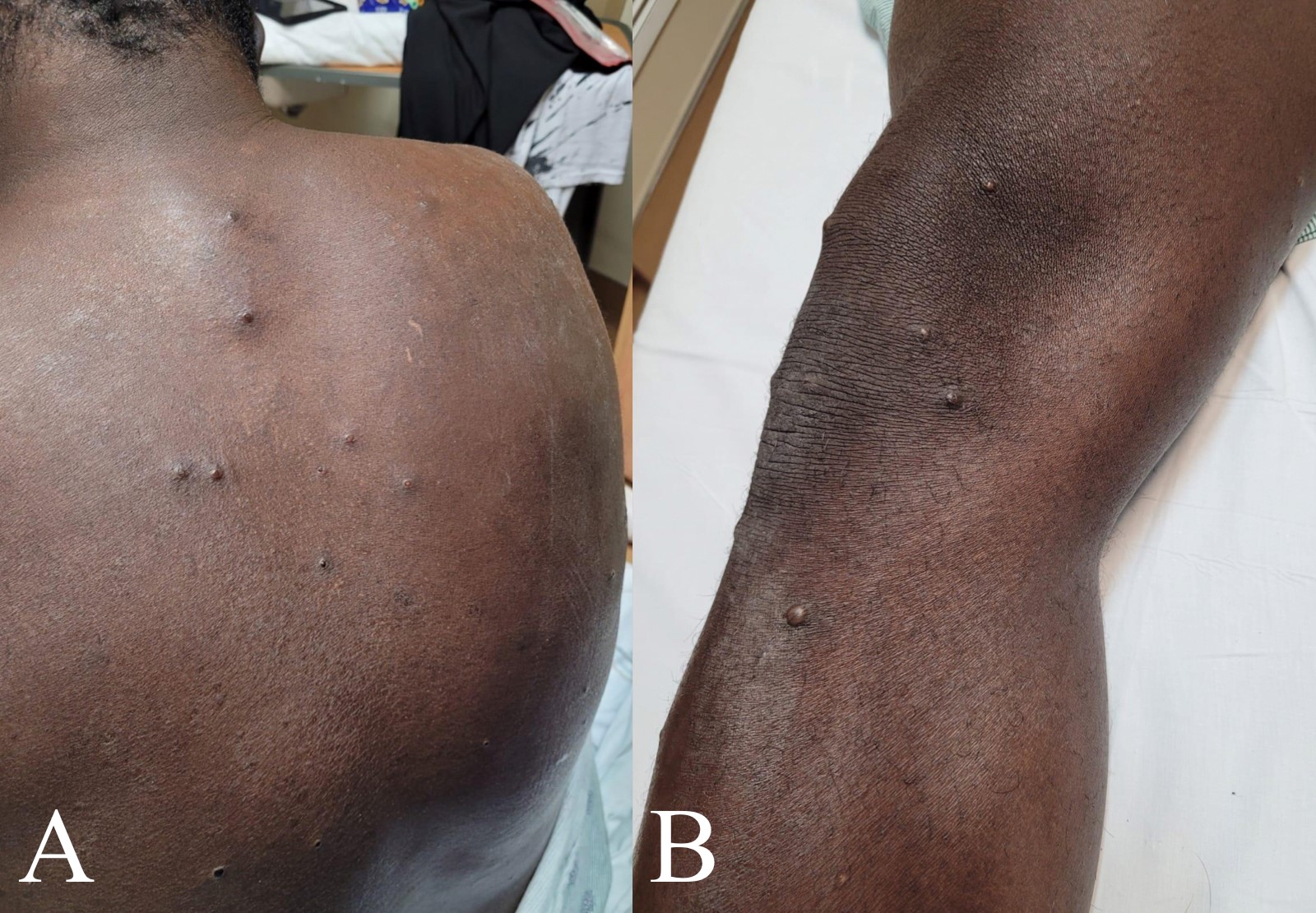 Figure 1: Vesiculopapular lesions on the back (A) and leg (B)
Figure 1: Vesiculopapular lesions on the back (A) and leg (B)
His HIV treatment regimen, consisting of an emtricitabine, rilpivirine, and tenofovir alafenamide fixed-dose combination tablet and dolutegravir, was continued during his hospital stay. The patient was otherwise treated with supportive care including IV fluids. His hospital course was uncomplicated and the patient experienced gradual desquamation of the vesiculopapular lesions. The patient was discharged nine days after initial ED presentation following desquamation of all of his lesions and the resolution of the monkeypox infectious period.
Discussion
To our knowledge, this is one of the first reported cases of COVID-19 and monkeypox co-infection in Florida and the United States more broadly. Our patient was immunosuppressed, with a history of intravenous drug use, current HAART therapy and coinfection with COVID-19, herpes and monkeypox. Even with these risk factors for severe complications of infection, our patient experienced an uneventful hospitalization. Our patient’s uncomplicated clinical course, along with the absence of monkeypox deaths in the United States to date, suggests a potentially less severe public health threat than originally predicted given the historical mortality rate around 10% in Central Africa where this virus originated and 3-6% mortality rate for the current strain [7-9]. While patients with monkeypox can present with severe symptoms, our case is an example of a patient with multiple comorbidities who presented with minor systemic symptoms, in addition to the vesiculopapular lesions characteristic of monkeypox infection.
Following a prodromal period of about a week, our patient presented with mild systemic symptoms and in no acute distress with widespread vesiculopapular lesions the primary manifestation of his monkeypox infection. As a result, supportive care along with airborne and contact precautions allowed for effective, timely management while minimizing risk of spread to medical staff. The patient was not given an antiviral treatment for monkeypox such as Tecovirimat or Brincidofovir as neither of these medications were approved for use in patients testing positive for monkeypox at the time of treatment. Likewise, he was not given monoclonal antibodies or other COVID-19 treatments due to the mildness of his respiratory symptoms and the need to hold HAART therapy during administration.
Conclusion
Our patient’s uncomplicated hospital course and seemingly mild presentation, even in the face of his use of immunosuppressive medications and coinfection with COVID-19, HIV and herpes, suggests the monkeypox strain currently in the United States may be less severe than once feared. While, vaccination and antiviral treatments for monkeypox have become available since the presentation of our patient, his case suggests supportive management may be adequate in future cases where these treatments are unavailable.
References
- Moore MJ, Rathish B, Zahra F (2022) Monkeypox. StatPearls. StatPearls Publishing, Treasure Island (FL).
- McCollum AM, Damon IK (2014) Human Monkeypox. Clin Infect Dis 58(2): 260-267.
- Bunge EM, Hoet B, Chen L, Lienert F, Weidenthaler H, et al. (2022) The changing epidemiology of human monkeypox-a potential threat? A systematic review. PLoS Negl Trop Dis 16: e0010141.
- Ennab F, Nawaz FA, Narain K, Nchasi G, Essar MY (2022) Rise of monkeypox: Lessons from COVID-19 pandemic to mitigate global health crises. Ann Med Surg 79: 104049.
- Quarleri J, Delpino MV, Galvan V (2022) Monkeypox: considerations for the understanding and containment of the current outbreak in non-endemic countries. Geroscience p. 1-9.
- Albrecht T, Almond JW, Alfa MJ, Alton GG, Aly R, et al. (1996) In: Baron S (Editors.), Medical Microbiology. (4rth Edition), University of Texas Medical Branch at Galveston, Galveston, USA.
- Bragazzi NL, Kong JD, Mahroum N, Tsigalou C, Khamisy-Farah R, et al. (2022) Epidemiological trends and clinical features of the ongoing monkeypox epidemic: A preliminary pooled data analysis and literature review. J Med Virol p.1-8.
- (2022) CDC updates U.S. monkeypox cases to 45, says overall risk remains low. American Hospital Association, USA.
- (2022) Monkeypox, WHO, Switzerland.
Citation: Knopp BW, Weiss HZ, Goldstein E and Parmar J (2022) Co-infection of COVID-19 and Monkeypox: A Case Report from Florida, USA, 2022. Curr Res Emerg Med 2: 1041

