International Journal of Orthopedics and Sports Medicine
[ ISSN : 2833-8375 ]
Neuromuscular Electrical Stimulation Increases Muscle Strength, Reduces Pain, and Improves Functional Recovery
Rubin Institute of Advanced Orthopedics, Rehabilitation Department, Sinai Hospital, Baltimore, MD, USA
Corresponding Authors
Mini Review
Muscle atrophy is considered to be one of the most prevalent underlying clinical conditions associated with knee osteoarthritis and in patients recovering from surgical procedures of the knee. Previous research has shown that patients can lose over 60% of their quadriceps strength after knee surgery, and in-clinic physical therapy programs alone may not be successful in restoring critical muscle activation strength [1]. In addition this loss of recovery is rapid and patients can lose up to 50% of the thigh volume in 1 month after surgery if the appropriate steps to reverse atrophy are not taken. In patients with pre-operative knee osteoarthritis, upper leg muscle strength is reported to be approximately 20–40% lower compared with healthy age-matched controls [2]. Thigh muscle weakness is strongly related to poor patient-reported outcomes, increased pain, activity limitations and falls, and has been linked to symptomatic progression of the disease. In addition, disuse atrophy and pain inhibition cause predominant weakness of the fast twitch muscle fibers. The fast twitch muscle fibers are responsible for many daily functions. These are larger diameter fibers and are quick to atrophy and harder to recover. There are four methods of fast twitch muscle recruitment 1) Blood flow restriction training (BFRT), 2) NMES maximally tolerated, 3) Max intensity eccentrics and, 4) Fast movement patterns such as limb perturbation or rhythmic stabilization. In a post-surgical patient only NMES therapy is safe in the early phase of recovery. Later on in the Rehab, NMES can be combined with BFR, followed by BFRT and then as the patient recovers in the later stage max intensity and fast movements and rhythmic stabilization can be incorporated.
Incorporating Neuromuscular Electrical Stimulation, or NMES therapy, to patient care pathway plans helps increase in thigh muscle strength and prevents further atrophy caused by knee osteoarthritis or after knee surgery. Neuromuscular Electrical Stimulation (NMES) is a neuromodulation technique that utilizes electrical stimuli to strengthen muscles through the increased recruitment of type II muscle fibers. NMES uses electrical muscle stimulation (EMS) to cause excitement in the muscle tissue. This is achieved by passing electrical impulses from a device through electrodes placed on the skin over the targeted muscles. The NMES stimulus is designed to mimic the same type of signal the brain sends to the muscle when exercising. In early stages of post-operative rehabilitation, NMES therapy is clinically useful modality to recruit and activate fast twitch motor units especially in the early phase of post-surgical recovery [3]. NMES is a safe, non-pharmacologic, and non-invasive modality to treat muscle weakness. By strengthening the quadriceps, NMES has the ability to correct imbalances and reduce additional stress on the joint, thereby potentially preventing atrophy and further strength deficits.
Neuromuscular Electrical Stimulation has been broadly researched for decades as a therapy option for post-operative rehabilitation and knee osteoarthritis. The use of NMES after total knee arthroplasty (TKA) has been demonstrated to facilitate quadriceps muscle recovery and increase overall quadriceps muscle strength [4-8]. One study showed the use of NMES for TKA is a promising method for improving patient outcomes, including significantly improved function and reduction in post-surgical pain, when home NMES units were used at least 40 minutes a day in addition to standard physical therapy 2-3 times a week for 1 hour (Table 1) [9]. Another recent study has shown that a home-based NMES device can improve patient function and allow for an earlier return to activity following TKA [10]. Several other studies have shown promising results with the use of NMES for knee osteoarthritis, leading to improvement in pain, muscle strength, exercise tolerance, and quality of life in patients with knee OA as well as those undergoing TKA [11-16].
Table 1: Independent samples t-tests comparing NMES home vs. control cohort Delanois et al. [9]
|
Pain and functional outcomes |
Experimental |
Control |
P |
|
Resting Pain |
2.73 (1.19) |
5.08 (2.43) |
<0.001 |
|
Worst Pain |
4.36 (2.18) |
6.69 (1.62) |
<0.001 |
|
Quad Lag |
10.38 (6.46) |
23.27 (8.71) |
<0.001 |
|
TUG |
12.45 (5.41) |
22.71 (8.88) |
<0.001 |
|
Single leg stance |
19.30 (10.77) |
7.67 (5.69) |
<0.001 |
|
Time to ascend/descend stairs |
22.88 (17.17) |
49.70 (26.36 |
0.001 |
|
2-mintues walking distance |
316.61 (151.26) |
260.83 (70.10) |
0.001 |
|
Active ROM: flexion (degree) |
94.38 (15.06) |
88.69 (15.80) |
0.19 |
|
Active ROM: extension (degree) |
7.31 (4.47) |
6.73 (7.34) |
0.734 |
|
Passive ROM: flexion (degree) |
104.19 (14.45) |
95.38 (15.23) |
0.037 |
|
Passive ROM: extension (degree) |
2.50 (4.06) |
|
|
There is a wide variety of NMES products available on the market-including plug in office systems as well as home-based battery-operated devices for single patient use. Each have important characteristics to consider when selecting an option for patient care plans, such as therapy effectiveness, ease of use, patient comfort, and accessibility throughout the rehabilitation period. One of the advantages of home-based units is that it can be used daily for a prescribed time per day. We recommend that patients use home-based units 40 to 60 minutes per day, with one session no more than 20 minutes. One of the notable at-home NMES devices on the market incorporates a smartphone app to control stimulation therapy and a specialized waveform for optimal therapeutic benefits. This specific product, the CyMedica e-vive System, is an US FDAcleared device allowing patients to access therapy from home, immediately after surgery. The device’s smartphone app is downloaded to the user’s smart device and allows the patient to control their stimulation sessions (Figure 1).

Figure 1: CyMedica e-vive NMES System.
The e-vive smartphone app also collects data points of patient progress such as therapy compliance, range of motion, pain levels, activity, and more. This app in-turn sends the performance data securely to an online cloud-based provider portal system allowing providers access through a standard web browser to monitor patient progress and take corrective actions in time. The device’s patented NMES waveform delivers an asymmetrical, complex, and monophasic shaped pulse to provide optimal therapeutic results while maximizing comfort and compliance (Figure 2). The unique design includes a longer pulse width (5 ms), monophasic polarity, work cycles, and regulated power output to provide a longer duration of muscle contraction within a 20-minute treatment session. The result is to provide a deeper activation of both type I and type II muscle fibers.
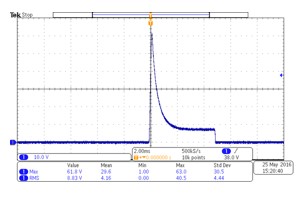
Figure 2: CyMedica patented NMES waveform.
The targeted muscle stimulation uses a closed-loop feedback system to regulate energy transferred to the patient, creating a comfortable experience for the user. Comfortable muscle stimulation, when performed at the maximally tolerated levels, can ultimately result in better patient compliance and success with therapy. Upon reviewing the currently available systems for NMES therapy, it is important to consider not only the therapeutic benefits, but also patient access, comfort, and ease of use-all of which can encourage a greater level of therapy compliance for optimal outcomes. A home-based NMES device is a non-invasive and non-pharmacologic treatment that patients can safely perform in the safety of their home to recover from post-surgical knee dysfunction as well as Knee OA. NMES home-based therapy should be an essential part of the continuum of care pathway in Knee OA as well as post-surgical Knee Rehabilitation.
References
- Mizner RL, Stephanie C Petterson, Jennifer E Stevens, Krista Vandenborne, Lynn Snyder Mackler (2005) Early quadriceps strength loss after total knee arthroplasty. The contributions of muscle atrophy and failure of voluntary muscle activation. J Bone Joint Surg Am 87(5): 1047-1053.
- Alnahdi AH, Zeni JA, Snyder Mackler L (2012) Muscle impairments in patients with knee osteoarthritis. Sports Health 4(4): 284-292.
- Toth MJ, Tourville TW, Voigt TB, Rebecca H Choquette, Bradley M Anair, et al. (2020) Utility of Neuromuscular Electrical Stimulation to Preserve Quadriceps Muscle Fiber Size and Contractility After Anterior Cruciate Ligament Injuries and Reconstruction: A Randomized, Sham-Controlled, Blinded Trial. Am J Sports Med 48(10): 2429-2437.
- Ulrich SD, Bhave A, Marker DR, Thorsten M Seyler, Michael A Mont, et al. (2007) Focused rehabilitation treatment of poorly functioning total knee arthroplasties. Clin Orthop Relat Res 464: 138-145.
- Bhave A, Mont M, Tennis S, Michele Nickey, Roland Starr, et al. (2005) Functional Problems and Treatment Solutions after Total Hip and Knee Joint Arthroplasty. J Bone Joint Surg Am 87: 9-21.
- Stevens Lapsley JE, Balter JE, Wolfe P, Donald G Eckhoff, Wendy M Kohrt (2012) Early Neuromuscular Electrical Stimulation to Improve Quadriceps Muscle Strength after Total Knee Arthroplasty: A Randomized Controlled Trial. Phys Ther 92: 210-226.
- Avramidis K, Strike PW, Taylor PN, Ian D Swain (2003) Effectiveness of electric stimulation of the vastus medialis muscle in the rehabilitation of patients after total knee arthroplasty. Arch Phys Med Rehabil 84: 1850-1853.
- Avramidis K, Karachalios T, Popotonasios K, Dimitrios Sacorafas, Athanasios A Papathanasiades, et al. (2011) Does Electric Stimulation of the Vastus Medialis Muscle Influence Rehabilitation After Total Knee Replacement? Orthopedics 34:175.
- Delanois R, Sodhi N, Acuna A, Doll K, Mont MA, Bhave A (2019) Use of home neuromuscular electrical stimulation in the first 6 weeks improves function and reduces pain after primary total knee arthroplasty: a matched comparison. Ann Transl Med 7(7): S254.
- Klika AK, Yakubek G, Piuzzi N, Calabrese G, Barsoum WK, Higuera CA (2020) Neuromuscular Electrical Stimulation Use after Total Knee Arthroplasty Improves Early Return to Function: A Randomized Trial. J Knee Surg.
- Chughtai M, Elmallah RD, Mistry JB, Anil Bhave, Jeffrey Jai Cherian, et al. (2016) Nonpharmacologic Pain Management and Muscle Strengthening following Total Knee Arthroplasty. J Knee Surg 29: 194-200.
- Chughtai M, Piuzzi N, Yakubek G, Anton Khlopas, Nipun Sodhi, et al. (2017) Use of an App-Controlled Neuromuscular Electrical Stimulation System for Improved Self-Management of Knee Conditions and Reduced Costs. Surg Technol Int 31: 221-226.
- Coquart JB, Grosbois JM, Olivier C, Frederic Bart, Ingrid Castres, et al. (2016) Home-based neuromuscular electrical stimulation improves exercise tolerance and health-related quality of life in patients with COPD. Int J Chron Obstruct Pulmon Dis 11: 1189-1197.
- Gwam CU, McGinnis T, Etcheson JI, Nicole E George, Assem A Sultan, et al. (2018) Use of Neuromuscular Electrical Stimulation During Physical Therapy May Reduce the Incidence of Arthrofibrosis After Total Knee Arthroplasty. Surg Technol Int 32: 356-360.
- Pal S, Chughtai M, Sultan AA, Anton Khlopas, Nipun Sodhi, et al. (2017) Impact of Neuromuscular Electrical Stimulation (NMES) on 90-Day Episode Costs and Post-Acute Care Utilization in Total Knee Replacement Patients with Disuse Atrophy. Surg Technol Int 31: 384-388.
- Mistry JB, Elmallah RD, Bhave A, Morad Chughtai, Jeffrey Jai Cherian, et al. (2016) Rehabilitative Guidelines after Total Knee Arthroplasty: A Review. J Knee Surg 29: 201-217.
Citation: Anil Bhave PT (2021) Neuromuscular Electrical Stimulation Increases Muscle Strength, Reduces Pain, and Improves Functional Recovery. Int J Orthop Sports Med 2: 1007

